JOINT INFECTION
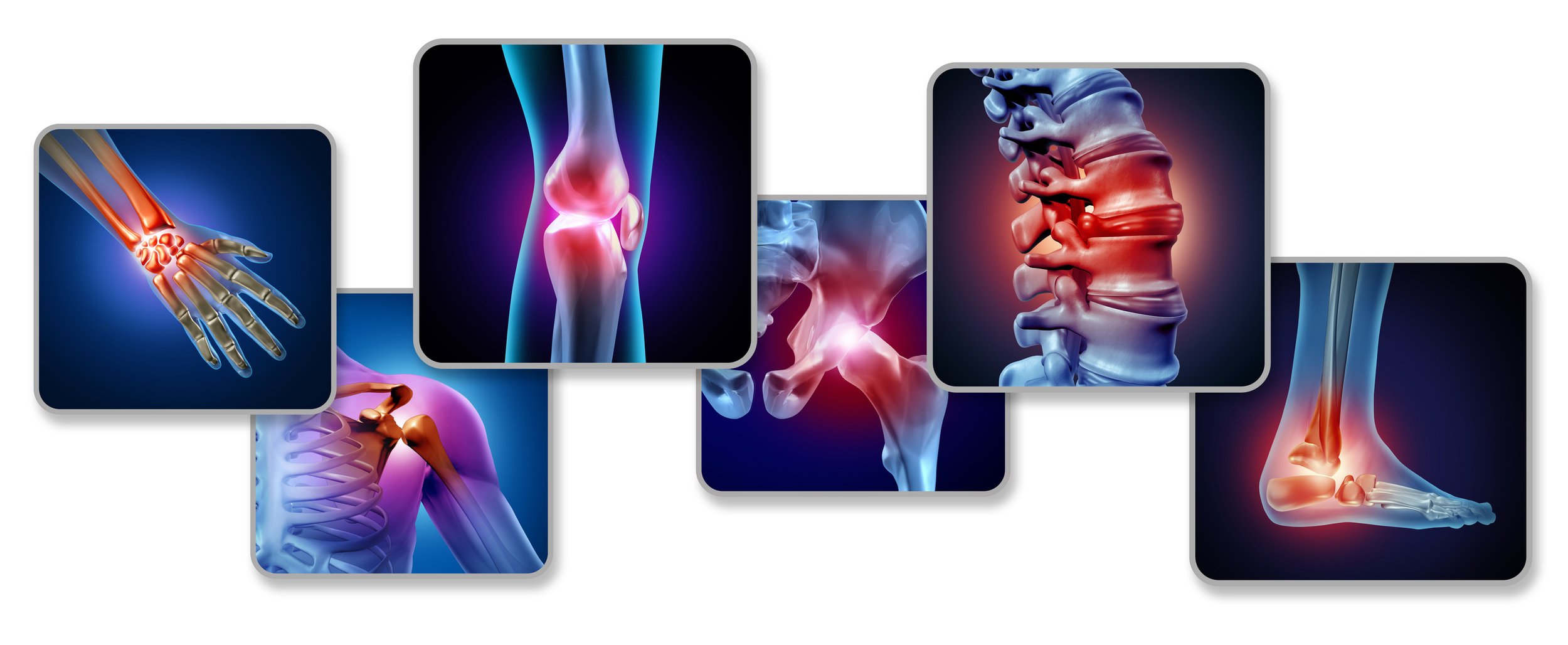
Joint infection, medically known as septic arthritis, occurs when bacteria, viruses, or fungi invade a joint, leading to inflammation, pain, and swelling. This condition can affect any joint in the body but is most commonly seen in larger joints, such as the knee, hip, and shoulder. Joint infections can arise from various sources, including direct infection from an open wound, the spread of bacteria from other areas of the body through the bloodstream, or post-surgical complications. Individuals with weakened immune systems, existing joint conditions, or those who have undergone recent joint surgery are at an increased risk for developing a joint infection.
Symptoms of a joint infection typically include severe pain in the affected joint, swelling, warmth, and redness over the joint area. Patients may also experience fever, chills, and difficulty moving the joint. Early diagnosis and treatment are crucial to prevent long-term damage to the joint and surrounding tissues. Orthopedic surgeons often perform joint aspiration, a procedure in which a needle is inserted into the joint to extract fluid for analysis, to confirm the presence of infection and identify the causative organism. Imaging studies, such as X-rays or MRIs, may also be utilized to assess joint damage and guide treatment decisions.
Treatment for joint infections generally involves a combination of antibiotics to eliminate the infection and supportive measures to relieve pain and restore joint function. In some cases, surgical intervention may be necessary to drain infected fluid or debris from the joint, particularly if aspiration alone is insufficient. Rehabilitation and physical therapy are often recommended post-treatment to aid recovery and restore strength and mobility. Timely intervention and appropriate management are essential to achieving favorable outcomes and preventing potential complications, such as chronic pain or joint deformity.
COMMON CONDITIONS
Septic Arthritis
Septic arthritis is a serious joint infection caused by bacteria, viruses, or fungi, typically resulting in severe inflammation and pain in the affected joint. The condition often occurs in the knee, hip, or shoulder, although any joint can be affected. Risk factors for developing septic arthritis include a weakened immune system, pre-existing joint diseases (such as rheumatoid arthritis), recent joint surgery, or intravenous drug use. Patients with septic arthritis typically present with symptoms such as intense joint pain, swelling, warmth, and redness, often accompanied by fever and chills. If left untreated, septic arthritis can lead to joint damage and long-term complications, including chronic pain and loss of function.
Orthopedic surgeons play a crucial role in the diagnosis and management of septic arthritis. Diagnosis usually involves joint aspiration to obtain synovial fluid, which is then analyzed for the presence of pathogens and white blood cells. Imaging studies, such as X-rays or MRIs, may also be used to assess joint integrity. Treatment often begins with intravenous antibiotics to target the infection, and in many cases, surgical intervention may be required to drain the infected joint and remove any purulent material. Early detection and comprehensive treatment are essential to prevent irreversible joint damage and facilitate a successful recovery.
Pediatric Septic Arthritis
Pediatric septic arthritis is a critical condition in children that involves infection of a joint, most commonly the hip or knee. It can result from hematogenous spread (infection spreading through the bloodstream) from other parts of the body, such as skin infections or respiratory tract infections. Children with septic arthritis often present with sudden onset of joint pain, fever, and reluctance to use the affected limb. They may exhibit signs of distress, and caregivers often notice swelling and redness around the joint. Early intervention is crucial, as untreated infections can lead to joint destruction and long-term disabilities.
Orthopedic management of pediatric septic arthritis typically involves both medical and surgical approaches. After a thorough clinical assessment and imaging studies to confirm the diagnosis, orthopedic surgeons may perform joint aspiration to obtain fluid for laboratory analysis and relieve pressure in the joint. If bacteria are detected, intravenous antibiotics are initiated immediately. In more severe cases, surgical drainage may be necessary to remove infected material and prevent complications. Rehabilitation following treatment is essential to restore normal function and mobility, emphasizing the importance of early diagnosis and comprehensive care to ensure optimal outcomes for pediatric patients.
COMMON PROCEDURES
Joint Aspiration (Arthrocentesis)
Joint aspiration, also known as arthrocentesis, is a minimally invasive procedure performed to diagnose and treat joint infections, such as septic arthritis. During this procedure, an orthopedic surgeon uses a sterile needle to withdraw fluid from the affected joint space. This fluid is then sent to the laboratory for analysis, where it can be examined for the presence of bacteria, white blood cells, and other indicators of infection. In addition to providing crucial diagnostic information, aspiration can also relieve pressure and swelling in the joint caused by excess fluid accumulation.
The procedure is typically performed under local anesthesia to ensure patient comfort. After cleaning the skin over the joint, the surgeon inserts the needle, and if fluid is present, it is carefully drawn out. In cases where a significant amount of infected fluid is removed, the surgeon may also inject corticosteroids to reduce inflammation and alleviate pain. Joint aspiration can often provide immediate relief from symptoms while simultaneously allowing for a rapid diagnosis. This quick and effective procedure is essential in managing joint infections and is frequently the first step in treatment.
Arthroscopic Debridement
Arthroscopic debridement is a surgical procedure that involves using a small camera (arthroscope) and specialized instruments to clean out an infected joint. This procedure is often indicated when joint aspiration alone is insufficient to manage a severe joint infection or when significant debris or infected tissue is present in the joint. During the procedure, the orthopedic surgeon makes small incisions around the joint and inserts the arthroscope to visualize the joint interior. They then remove infected tissue, debris, and any damaged cartilage, which helps restore normal joint function and reduce the risk of complications.
Arthroscopic debridement is performed under general or regional anesthesia, depending on the patient's needs and the joint involved. Postoperatively, patients typically undergo rehabilitation to regain strength and range of motion in the joint. This procedure can significantly improve outcomes for patients suffering from septic arthritis or other joint infections, allowing them to return to their normal activities more quickly. Early intervention through arthroscopic debridement can prevent long-term joint damage and promote better healing, making it a valuable option in the treatment of joint infections.
